In This Article, we will give a general idea about Human Herpes virus (HHV) and a Detail description about the Hepres Simplex Virus, Pathogenesis, Clinical Features, Diagnosis, Types and Treatment.
Herpes Virus
Facts
- The Name Herpesvirus is derived from the greek word herpein, which means to creep, as the virus tends to creep back or return as they have the ability to remain latent in a viable form within the host sell after the primary infection. They may be latent ant persist for a long time and reactivate in certain condition ( stress, low immunity …etc), to infect again producing a recurrent form of infection.
- They are identical morphologically.
- They Are Double Stranded DNA Virus.
- Replication is done by nuclear-replicating, the viral DNA is transcribed to mRNA within the infected cell’s nucleus.
- Effects both animals and humans, but are divided into 8 types that infect humans HHV (Human Herpes Virus)
- HHV-1 :Herpes Simplex Virus 1
- HHV-2 :Herpes Simplex Virus 2
- HHV-3 :Varicella-Zoster Virus
- HHV-4 :Epstenin-Barr Virus
- HHV-5 :Cytomegalovirus
- HHV-6 :Herpes lymphotropic virus (Roseolovirus)
- HHV-7 :Pityriasis Rosea
- HHV-8 :Kaposi’s sarcoma-associated herpesvirus
Herpes Simplex Virus
Features
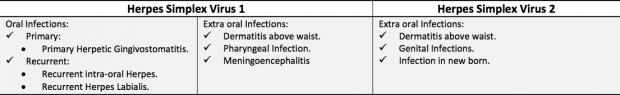
- There are two types of Herpes Simplex Virus Type 1 and Type 2.
- Type 1 which produce oral lesions (Cold sores) while Type 2 mostly produces Genital Lesions, This doesn’t mean that Type 1 can’t effect the genital area through oral sex and Vice versa.
- They Are very contagious.
- Basic symptoms are blisters on the skin or mucosal membranes.
- They neurotropic virus, as they capable of infecting nerve cells and become latent in the neuron bodies hidden away from the immune cells.
Herpes Simplex Virus 1
- Human herpes virus 1 (HHV1) is also known as herpes simplex virus 1 (HSV1).
- It is typically the cause of cold sores around the mouth.
- HHV1 can also lead to infection in the genital area causing genital herpes usually through oral-genital contact, such as during oral sex.
- HHV1 infections are contagious and are usually spread from skin-to-skin contact with an infected person through small breaks in the skin or mucous membrane. The HHV1 virus is more likely to be spread through things like sharing eating utensils, razors, and towels from a person who has an active lesion.
Herpes Simplex Virus 2
- Human herpes virus 2 (HHV2) is also called herpes simplex virus 2 (HSV2).
- It typically causes genital herpes, a sexually transmitted infection. However, it can also cause cold sores in the facial area. Like HHV1, the HHV2 infection is contagious and is spread by skin-to-skin contact. The main route of transmission is through sexual contact, as the virus does not survive very long outside the body.
- In case of newborns, the infections are due to the contact of the infant during delivery with a vaginal lesion of the mother. Most infants are asymptomatic but in some minority may show manifestation by the 4th to 7th day (Jaundice, Hepatosplenomegaly,Thrombocytopenia and large vesicular lesions on the skin) and with a high mortality rate by the 9th to the 12th due to viremia.
- In Case of Adults, Primary infection as Genital lesions is rare but may start to increase after the age of 14, due to increase sexual activity.
Sites
Difference
- They are Virtually identical sharing 50% of their DNA.
- Both Infect The oral muscoa, skin and genital areas and are latent in the nervous system.
- Both have recurrence and are easily spread.
- Both have similar clinical features causing a Herpes Simplex Infection.
- The Main difference is where Virus prefers to stays latent:
- HSV1 prefers the the trigeminal ganglion where it recurrence occurs in the lower face and lips.
- HSV2 prefers the the sacral ganglion where it recurrence occurs in the genital area.
- But this preference isn’t absolute as either can interchange and occur in each other’s preference (HSV1 can be in the genital area and Vice Versa).
One type is associated with stigma, the other is “‘just a cold sore”- our society has a euphemism for it so we don’t even have to acknowledge that it’s herpes.
Herpes Simplex Infections
Types
Primary Herpetic Infection
Occurs By Primary Infection
No Prior Immunity (AB Raise by Convalescene)
Local and Systemic Manifestations
Examples
Herpetic Gingivostomatitis
Herpetic Whitlow
Recurrent Herpetic Lesion
Occurs by activation of latent Virus
High Antibody Titre
Local manifestions with NO systemic features
Examples
Hepres labialis
Intra-Oral Herpes
Primary Herpes Infections
We will start with the Primary Type of Herpes Infection, While the Recurrent Type of Herpes infection will be tackled in the next Article.
Acute Herpetic Gingivostomatitis
Features
-
Primary Herpes In a Child Common in children (1 – 10 years old) and highest peak at 2‐3 years.
- Uncommon in adults and infants younger than 6 months, why? Because the infant acquires the IgG (maternal AB)that pass the placenta from the mother and life span of the antibody is 6 months.
- In case of children, 95 – 99% of cases run Subclinical and may be misdiagnosed as Teething; while 1 – 5% of cases exhibit the clinical course of the disease.
- In case of adults, the manifestations aren’t typical: shorter duration, fewer oral ulcers and less pronounced systemic manifestations.
- Antibody Titre:
Pathogenesis
- Intraepithelial vesicles due to destruction of the prickle cell layer.
- Presence of Multinucleated Giant cells in the epithelial cells lining the vesicle due to fusion of the infected cells with normal cells or division of the infected cells’ nucleus without the division of the cytoplasm.
- Presence of nuclear Inclusion bodies in the infected epithelial cells (Lipschutz Bodies).
- The Nucleus appears homogenous with migration of chromatin (Ballooning degeneration)
Duration
- Self Limiting and disease course is 10 – 14 days, but the duration tend to be less in adults.
- Disease course is more severe in:
- Premature and newborns infants.
- Malnourished and immune‐compromised patients (immune suppressive drugs or malignancy or severe burns).
Clinical Features
Prodrome
Occurrence: Precedes the lesions by 1‐2 days and subsides within 3 days.
Fever, headache, malaise, nausea, vomiting and refusal of feeding.Submandibular and upper deep cervical lymph nodes Lymphadenopathy (Tender and palpable)
Acute Marginal Gingivitis
Occurrence : 1‐ 2 days after prodrome
Acute inflammation of the gingiva with bleeding and edema and persist during the whole course of the disease.
The oral lesion appears as ulceration and erosion of the gingiva (due to the rupture of the vesicles) BUT there is no losing of marginal gingiva or Interdental papillae. A Crucial Difference for ACUTE NECROTIZING ULCERS.
Vesicular eruptions
Once the fever subsides, vesicles start to erupt in the oral cavity and circumoral tissue (vermillion board of the lip) and circumoral skin. These vesicles appear on the both keratinized and non‐keratinized mucosa.
These vesicles may coalesce to form a bullae with irregular outline, this is due to: Humidity, mechanical irritation and high temperature.
Vesicular Rupture and ulcer formation
These vesicle may rupture giving A shallow erosion or ulcer they are Small and round, Surrounded by an inflammation and Covered by grayish membrane.
This ulcer may coalesce to form a larger ulcer.Theses Ulcers are painful Excessive Salivation (Pain reflex) –> Saliva is filled with Viruses –> the saliva is infective –> infecting the lips or hands and may even spread to the eye (Conjunctivitis) and genitals (Vulvovaginitis).
Diagnosis
History
Prodrome preceding oral lesions.
History of contact of lesion either primary or recurrent with other infected people. No history of recurrent lesion within the same person.
Clinical Examination
Gingival inflammation.
Lymphadenopathy.
Ulcer formation after vesicular eruption.
Special Investigations
Only preformed when the patient has no obvious clinical manifestations.
- Cytological Smear from unruptured vesicles nucleus with Geimsa StainGiant cells and Inclusion bodies. o Isolation of HSV in tissue cultures (e.g. Rabbit’s Kidney).
- Total leukocytic count (either normal or elevated)
- Antibody Titre:
Treatment
Treatment is mainly Supportive and symptomatic treatment, why? Because it’s a self limiting disease.
- Bed Rest.
- Supportive therapy (liquid diet with proper calories and high nutritional value to raise the body resistence. Pain relief by analgesics and topical anesthetics.
- Antipyretic. (Paracetamol)
- Orabase to protect the ulcer during healing (Sodium carboxymethyl cellulose)
- Antibiotics, why? Use Broad spectrum to prevent 2nd bacterial infections.
- Antiviral drugs, only used when In severe cases or In immune‐compromised patients or If the disease is disseminated.
Herpetic Withlow
Features
- Primary Herpetic Infection.
- Infection on the fingers due to occupational Hazards ( most commonly in doctors, dentist or nurses that contact patients that have a herpetic lesions)
- A finger injury is needed for the disease to occur and exposure to an oral or pharyngeal herpes infections.
- ITS ALWAYS RECOMMENDED: Use both Rubber dam and gloves are essential means for protection.
Clinical Features
- Locally: Inching and pain on the infected finger.
- Systemic: May Manifest if the patient is seronegative ( That the Antibody against herpes isn’t present in the body, No Prior exposure before).
- Deep vesicles my coalesce in the distal segment of the finger.
- Self Limiting and heals within 18 – 20 weeks.
- Incision of the vesicle may complicate the lesion into a more serious problem (secondary bacterial infection or encephalitis)
Sources
- C-Health.
- Misr International University Article written By Dr. Mohsen S. Mohamed.
- Wikipedia.
- Herpes.
OziDent Members Only
The rest of article is viewable only to site members,Please Register and/ or Confirm registration via EmailHere.If you are an existing user, please login.